
Cancer isn’t a cops-and-robbers medical story in which a bad guy gets identified and vanquished, like in stories of smallpox, cholera, or scurvy.
Cancer is a criminal syndicate. We make the occasional collar, but we’re nowhere close to busting up the ring. Countless accomplices remain at large, playing roles we don’t fully understand.
Have a look at the rap sheet on prostate cancer.
Street-level bust
In any raid, the perp fingered first is the bottom guy, the one on the street.
For us, that was testosterone.
Two decades after collaring T, scientists discovered who T answers to: the androgen receptor.
Though the AR is nowhere near the top of the heap, it remains the biggest player we’ve got, and we squeeze it for all its worth.
Testosterone deprivation is one kind of squeeze. Enzalutamide and related drugs are another,1 and the search continues for more.
The androgen receptor is a big deal. Once you make sense of it, you can make sense of an enormous amount of prostate cancer research.
Unlucky dogs
First, though, let’s get back to testosterone.
We hear that Huggins and Hodges discovered androgen deprivation in the 1940s, but it’s not often explained what made them think of it.
One way for scientists to determine an organ’s function is to remove it and observe what happens. As you're aware, the testicles are an organ whose removal is frighteningly easy.2
Some unfortunate dogs showed 19th century researchers that castration leads to prostate shrinkage. Huggins speculated that this might be an inroad to prostate cancer, and experimented with dogs before his groundbreaking demonstration in the 1940s that testosterone deprivation shrank metastases in humans.3
As with many treatments, doctors didn’t know why it worked.
But they knew where to look. Testosterone is a hormone, a hormone is a signal, and a signal needs a receiver. In the 1960s, three researchers independently identified the receiver for testosterone — the androgen receptor.
Hearing its name, you might not visualize what the androgen receptor is. It’s a molecule. There are tens to hundreds of thousands of androgen receptors in a cell, and they’re found not just in the prostate but in cells throughout the body.4
Tailgaters
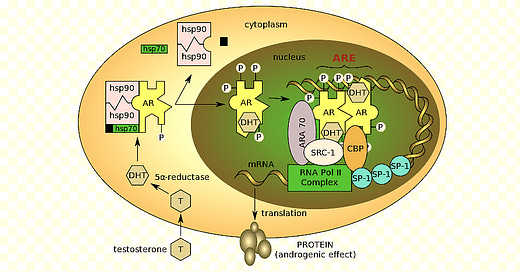
Here’s where testosterone and the AR meet. Testosterone reaches a cell from the bloodstream and binds to an idle AR molecule inside. This activates the AR.5
The AR is a transcription factor. The job exists because DNA is only a blueprint6 — other molecules need to unroll it and still others are needed to build from it. The transcription factor gets the job started.
It binds to the DNA at a gene-specific location and helps recruit a molecular team of coregulators to get transcription underway. The identity of these coregulators may vary from gene to gene, but the transcription factor is always the guy whose back they stand on.
AR ties in with PSA — the gene that expresses PSA is one of the genes that AR is a transcription factor for.7 In a healthy prostate we see a low PSA; when PSA climbs, we’re seeing the androgen receptor working overtime.
AR performs its cancer gig with perfect deniability. It’s doing what it always does. Cancer has turned the AR into a patsy, tricked into enabling cancer genes along with AR’s usual crew.
It’s not at all clear which genes the bad ones are or how they get there. They might be mutants, or perhaps they’re just the wrong genes at the wrong time.8
In principle, doctors at this point can move up the criminal chain — find the locations in DNA where AR attaches and identify the bad genes.
The unhappy news is that the AR is a transcription factor for hundreds or thousands of genes, and we’re far from identifying the bad ones.9 In the kind of desperation move we often see in cancer treatments, we squash the AR to stop the cancer genes, but that also squashes the genes that AR should normally be transcribing. ADT side effects are the result.
Recap
To summarize: Testosterone switches on the AR; the AR plays a key role in expressing certain genes; it gets duped into helping express genes that cause prostate cancer. Because we can’t identify those genes — much less block them — we try to shut down the entire androgen receptor. Since testosterone is the receptor’s ON switch, androgen deprivation is one way to do this. There are also drugs like enzalutamide that have several ways to keep the AR from doing its job.
As we know, the AR eventually wriggles free of all of attempts to keep it down, and stays active throughout the course of most prostate cancers. So researchers continue to investigate novel ways to stop it.
That’s the basics, but there are lots of colorful details.

Oily charm
Testosterone is derived from cholesterol, so it’s like an oil drop in the body’s aqueous environment. It drifts unimpeded through the cellular membrane, which keeps watery solutions out.
Initially AR is clutched by a number of chaperone molecules — that’s the term — but these chaperones want a hookup to take place; they position the AR to interact with testosterone floating past. The testosterone and AR then bind and travel as a unit; the chaperone molecules float away. Switched on, the AR starts its cancer mission.
Nuclear escort
Recall that a cell’s DNA is in its chromosomes, and the chromosomes are in the nucleus. To protect DNA from random crazy molecules that could damage it, access to the nucleus is tightly controlled. Molecules must be escorted in.
A section of the AR works like an employee badge. Seeing it, transporter molecules ferry the AR toward the nucleus and through the nuclear membrane.
Once inside, the AR finds another AR molecule to bind to, forming a molecular twin known as a dimer. These will work together.
Onto the DNA
Here is an AR dimer filling its role of transcription factor:

The DNA binding domains (DBD) are resting on the DNA. The black rows represent the two strands of the DNA helix, and the letters show a DNA code that AR will bind to.10
A ligand — possibly testosterone, but here DHT11 — is bound to the ligand binding domains.
The hinges are helping keep the AR positioned.
The N-terminal domains (NTD) on the outside provide binding access to other molecules that will participate in transcription.
Promoters, enhancers, and a backbend

And here’s a second bit of acrobatics.
Associated with each gene is a patch of DNA called the promoter, where a transcription factor and its transcription collaborators (called coregulators) gather to kick off that gene’s transcription. This DNA patch is usually found right before the gene.
But many genes also rely for transcription on a distant second site, the enhancer. The chromosome actually backbends, as in the figure, so the transcription molecules on the enhancer will contact those on the promoter.
The AR typically binds to an enhancer (see the red AR at the top) rather than a promoter. The promoter in the figure is at the bottom, where the red arrow marked TSS (transcription start site) shows the start of the gene being transcribed.
Recall that DNA in chromosomes is wrapped around proteins called histones, which appear here as disks. Only unwrapped DNA can be transcribed, and you see in the figure an unwrapped enhancer, promoter, and gene.
There’s more to the story
Though you’ve surely heard enough, the story has further chapters that we won’t go into. Some testosterone activity doesn’t involve the androgen receptor, and the androgen receptor can serve in roles other than transcription factor. The testosterone-AR connection is the one you’ll see in prostate cancer papers.
Patients who go on monotherapy — discontinuing Lupron and taking only an anti-AR drug like enzalutamide — report feeling better, and testosterone’s non-AR roles may be a reason.
And more to come
Understanding the structure and function of the AR enables you to understand much of our current and future treatment. Later posts will look at AR-targeting drugs — current ones like the lutamides, and investigational ones like PROTACs and N-terminal domain inhibitors. Doctors continue to search for vulnerabilities in the AR and beyond it.
The lutamide drugs — enzalutamide, apalutamide, darolutamide — all target the AR directly, and in similar ways, but the details are a subject for a later post. Notice abiraterone isn't on that list — it’s a different beast that blocks testosterone production.
The removal is also nonfatal, a plus for this kind of study.
Remember that metastasis is the name of the game here. If prostate cancer hasn’t metastasized, you can just remove the prostate. No Nobels are given for that. Huggins won the Nobel Prize in 1966 for ADT. Even the earliest subjects who felt squeamish about castration could take a drug instead — estrogen — but then faced potentially lethal side effects. In 1977 a relieved Nobel jury awarded the prize to Andrew Schally for finding a much safer alternative — essentially, Lupron.
Other hormones have receptors of their own— progesterone receptors, glucocorticoid receptors, and so on. So we say the androgen receptor meaning it’s the androgen receptor and not one of those other receptors.
Why not the testosterone receptor? Testosterone is the heart of why it exists, but the AR can also respond to similar molecules. Collectively these are called androgens. Roughly speaking, an androgen is a male sex hormone, though women have androgens too.
The testosterone that to us is the elixir of life is, to cancer, just an errand boy who pushes a button.
The post Genes? Chromosomes? DNA? describes the workings of DNA and transcription.
Or AR can work as a transcription repressor, silencing genes that would prevent cancer if left alone.
That’s not all. You may remember that DNA is tightly coiled to prevent expression of most genes, and that only uncoiled areas can be expressed. So maybe genes are unchanged, and it’s bad uncoiling that puts the wrong genes in the AR’s path. An alteration that changes gene expression without changes to DNA is called epigenetic.
ARs bind to specific sequences in the DNA. The A, G, C, T in the figure represent, of course, the DNA nucleotides adenine, guanine, cytosine, and thymine. The (NNN) in the figure means “any three nucleotides.”
A sequence that the AR will bind to is called an androgen response element (ARE).
The response element in the picture is a little puzzling. Since the ARs are sitting face-to-face, you’d think the letters on the right should be the reverse of the letters on the left. That’s often true, but the literature also shows this example. Biology is full of stuff like this.
Some testosterone entering the cell is converted to the androgen DHT (dihydrotestosterone), and like testosterone it binds to the AR and turns it on.



Thank you, Jim!
Ben, As always - Thank you for your research and clear (although I will need to read this numerous times) prose explanation with cool pictures. No wonder my PCa treatment is so perplexing and makes me sleepy trying to know what to do, when to do it, and what recommendation to follow.
Jeff